Assessing the level of consciousness and establishing a prognosis for recovery of consciousness in patients who are behaviourally unresponsive are fundamental shortcomings of clinical practice. Significant progress has been made in the neuroscience of consciousness, resulting in highly accurate diagnostic and prognostic indices in patients with a disorder of consciousness. However, the majority of these indices rely on specialized technologies that are challenging to integrate into everyday clinical environments. The BIAPT lab is working on developing the Adaptive Reconfiguration Index (ARI) – a translational index that overcomes this problem.
The healthy brain functionally reconfigures in an organized manner as it loses consciousness in response to propofol, a widely used general anesthetic. The ARI is based on the hypothesis that unresponsive, brain-injured patients who undergo similar brain network reconfigurations in response to propofol have the capacity to recover consciousness.
Electroencephalography (EEG) measures the electrical activity of cortical neurons using scalp electrodes. It is significantly less expensive than other imaging technologies, has fewer patient contraindications, and can be used at the bedside. Using EEG, the ARI measures the brain’s response to a neurophysiological perturbation by propofol anesthesia.
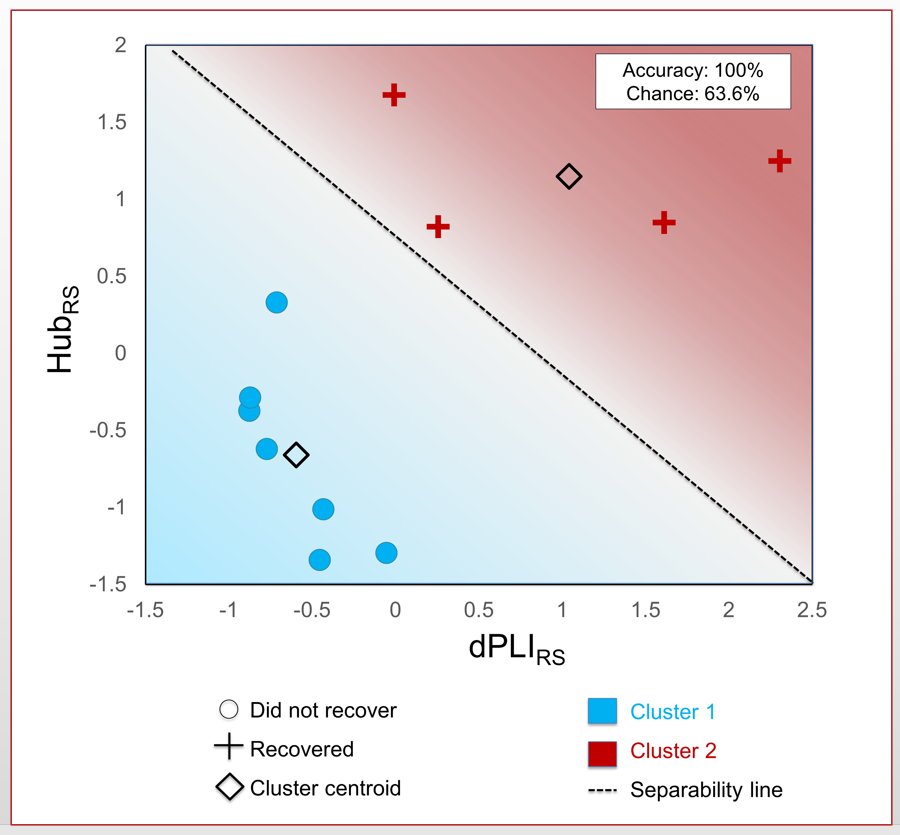
In an initial study with 12 patients in acute and chronic disorders of consciousness, the ARI was able to predict with 100% accuracy which patients were able to recover consciousness within 3 months. This predictive accuracy was held across a high-density, 128-channel EEG system and an 18-channel EEG, which is typically available in Western intensive care units.
The ARI overcomes the limitations of existing methods of DOC prognosis. EEG and propofol anesthesia can be administered at the bedside with no patient distress or contraindications, affording the ARI tremendous translational potential for acute clinical settings. The approach is independent of the patient’s capability for or willingness to react to external stimuli or commands. The ARI performed equally well across acute and chronic DOC, and across patients with various aetiologies of brain injury, suggesting its applicability across diverse brain-injured populations.
The BIAPT lab is currently:
- Validating the ARI in a larger sample of patients in a disorder of consciousness recruited from across Canada. This project is supported by a mentored research award granted to Dr. Catherine Duclos from the International Anesthesia Research Society (IARS).
- Adapting the ARI to pediatric patients in a disorder of consciousness.
Presentation of the ARI received the Best of Clinical Science Abstract prize at the 2019 Society for Neuroscience in Anesthesiology and Critical Care (SNACC) Meeting, and earned Dr. Blain-Moraes the 2020 Women in Neuroanesthesiology and Neuroscience Education and Research (WINNER) award from SNACC in recognition of contributions to neurosurgical anesthesia and for outstanding scientific research.
This project is supported by the Canadian Foundation for Innovation. It is currently being led by Dr. Catherine Duclos and Charlotte Maschke.